Cannabis for Glioma Brain Cancer
Can Marijuana Help People with Glioma Brain Cancer? from CannabisNet on Vimeo.
Glioma is a kind of tumor that develops in the brain and spinal cord. They occur in the supportive cells, also known as the glial cells, that surround nerve cells and are essential for healthy functioning.
There are three different kinds of glial cells, all of which can produce tumors. These are:
- Astrocytomas (astrocytoma, anaplastic astrocytoma and glioblastoma)
- Ependymomas (anaplastic ependymoma, myxopapillary ependymoma and subependymoma)
- Oligodendrogliomas (oligodendroglioma, anaplastic oligodendroglioma and anaplastic oligoastrocytoma)
The symptoms of glioma will vary depending on the kind of tumor as well as its location, size, and speed of growth. Common signs and symptoms include: headaches, vomiting, nausea, decline in brain function, confusion, memory loss, difficulty with balance, urinary incontinence, personality changes, irritability, vision problems, speech difficulties, and seizures.
Gliomas are also assigned various grades depending on its potential to grow, and how aggressive it is. Tumors are grade I to V, where grade I is the least serious kind of tumor while grade V is the most serious. Generally, gliomas are referred to as low grade or high grade. Usually, high grade or extremely aggressive gliomas develop their own blood supply. They are so aggressive that they can break down the blood-brain barrier in the area near the tumor, and can even grow back after surgical removal. For this reason, they are referred to as recurrent brain cancer.
The prognosis for patients with high-grade gliomas are generally poor, particularly for older patients.
How Cannabis Helps
Scientific research shows that various cannabinoids in the cannabis plant can help brain cancer patients in many ways:
Cannabis Induces Cancer Cell Death
A 1998 study whose results were published in the journal FEBS Letters showed promising results. The study, conducted by researchers from Madrid’s Complutense University, School of Biology, found that delta-9-THC induced apoptosis (programmed cell death) in glioma cells in culture. The researchers followed up their findings in 2000, and reported that administering both THC as well as the synthetic cannabinoid WIN 55,212-2 “induced a considerable regression of malignant gliomas” in animal models. In 2003, the same researchers also confirmed that cannabinoids have the ability to inhibit tumor growth in animal models.
In 2003 as well, Italian researchers from the University of Milan, Department of Pharmacology, Chemotherapy and Toxicology reported that CBD worked in inhibiting the growth of human glioma cell lines in vivo (cells studied inside the body) and in vitro (cells studied outside the body). They reported their findings in the November 2003 issue of the Journal of Pharmacology and Experimental Therapeutics Fast Forward, saying: “Non-psychoactive CBD… produces a significant anti-tumor activity both in vitro and in vivo, thus suggesting a possible application of CBD as an antineoplastic agent.”
Another study conducted in 2014 by Wai Lu, an oncologist at St. George’s University in London found that cannabis is promising in destroying glioma cells. Lu discovered that the primary cannabinoids THC and CBD alone were already beneficial in eliminating almost half of the glioma cells in affected animal models. Additionally, they found that when the cannabinoids were used together with radiotherapy, the treatment caused the tumors in many animal models to stop growing completely. Lu and his team also found that when CBD and THC were used together, they were able to achieve the same effects when less of each compound was used. Lu thinks that the reason behind the success of the cannabinoid treatment lies in neural pathways used for radiotherapy. “We think that the cannabinoids are hitting a number of cell signaling pathways, which primes them to the effects of irradiation,” he says. What’s amazing about this study is it reveals even if THC and CBD kill glioma cells, they don’t have any negative impact on the healthy cells surrounding glial cells.
Cannabis Prolongs Lives Of Brain Cancer Patients
An early 2017 study conducted by GW Pharmaceuticals analyzed 21 patients with recurrent glioblastoma multiforme. All patients were taking conventional cancer therapies, and they were then given either a cannabis extract containing THC and CBD, or a placebo.
“Patients with documented recurrent GBM treated with THC:CBD had an 83% one year survival rate compared with 53% for patients in the placebo cohort,” GW Pharma said in a press release. “Median survival for the THC:CBD group was greater than 550 days compared with the 369 days in the placebo group.”
“The findings from this well-designed controlled study suggest that the addition of THC and CBD to patients on dose-intensive temozolomide produced relevant improvements in survival compared with placebo and this is a good signal of potential efficacy,” writes Professor Susan Short, PhD, a lead author of the study.
“We believe that the signals of efficacy demonstrated in this study further reinforce the potential role of cannabinoids in the field of oncology and provide GW with the prospect of a new and distinct cannabinoid product candidate in the treatment of glioma,” says GW Chief Executive Officer Justin Gover.
OTHER STORIES YOU MAY ENJOY...
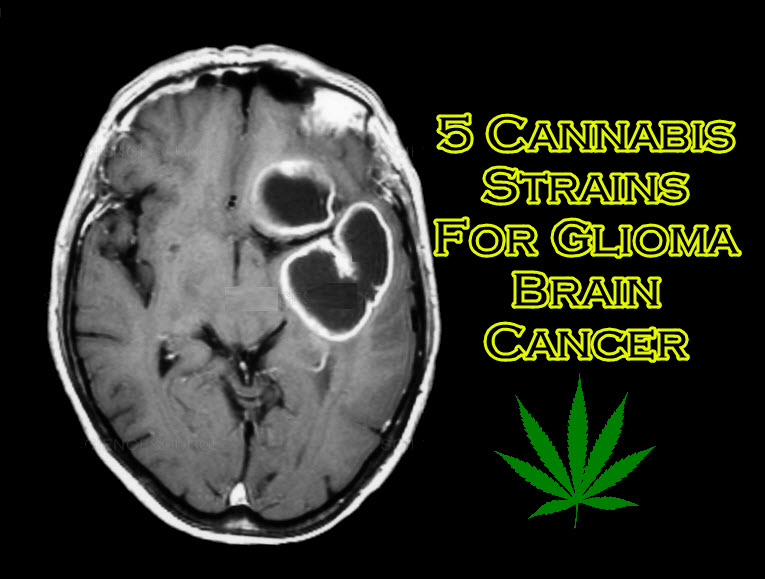
CANNABIS STRAINS FOR BRAIN CANCER, CLICK HERE.
OR...
CANNABIS TBI RESEARCH, CLICK HERE.
OR..
THE BRAIN AND CANNABIS HEALING, CLICK HERE.